Descriptions of surgeries
(for reference only, no appointments can be made without prior consultation!)Surgical Treatment of Lumbar Disc Prolapse (Hernia)
Introduction
Statisticians estimate that approximately 80 % of all population experience at least once a pain of lumbago type and approximately 50 % of population is severely affected by an attack of the pain at least once in their life. An average age at which the problems start is 27 years, and in 35 % of thus affected persons a typical lumboischiadic syndrome (LIS) develops within 10 years from the first attack. Severe LIS characterized by pain in the lumbar spine area with limited motility and typical pain-shooting to the lower limb affects about 2-3 % of population, a half of which is caused by changes in an intervertebral disc.
It is a typical civilization disease caused by mostly sedentary work. Impaired functions of abdominal, gluteal and spinal muscles along with frequent overweight result in development of abnormal movement stereotypes and overcharge of the spine, which creates conditions for development of lumboischiadic syndrome.
Anatomical and Pathophysiological Notes
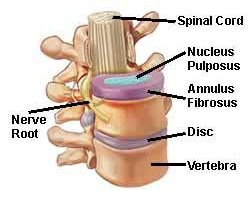
The basic structural element of the spine is a movement segment that consists of an intervertebral disc
and two intervertebral joints. The disc joins two vertebral bodies, is of an oval shape with a diameter
of 30 mm and height of 8 mm. On its circumference there is a ring with solid concentric collagen fibres
- anulus fibrosus, inside which there is a jellylike core - nucleus pulposus with a high content
of fluid. To the vertebral body a vertebral arch is attached from which articular processes and spinous processes
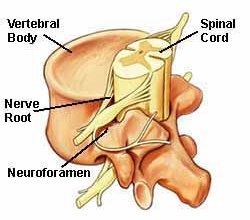 protrude. The firm connection via ligament defines the spinal canal, a tube going along the whole spinal
column. The spinal canal contains dura mater filled with liquid - cerebrospinal fluid. Spinal cord reaches
the second lumbar vertebra, which give up to nerve fibres towards the sacrum. They join in spinal nerves
that come out in couples to the left and to the right at the level of discs from the spinal canal through
small intervertebral apertures - intervertebral foramina. At the level of a disc, an anterior third
of the spinal canal, which has a diameter of 15 to 20 mm in the lumbar region, is formed by the posterior
part of vertebra; lateral and posterior walls are defined by bone and ligament parts.
protrude. The firm connection via ligament defines the spinal canal, a tube going along the whole spinal
column. The spinal canal contains dura mater filled with liquid - cerebrospinal fluid. Spinal cord reaches
the second lumbar vertebra, which give up to nerve fibres towards the sacrum. They join in spinal nerves
that come out in couples to the left and to the right at the level of discs from the spinal canal through
small intervertebral apertures - intervertebral foramina. At the level of a disc, an anterior third
of the spinal canal, which has a diameter of 15 to 20 mm in the lumbar region, is formed by the posterior
part of vertebra; lateral and posterior walls are defined by bone and ligament parts.
In the beginning, till the age of 16, the intervertebral discs are nourished by vessels that gradually die, and then the only nourishment and potential repair is ensured by limited penetration of molecules through cover plates, mostly at night when the conditions are the most suitable for diffusion, because while the body is sleeping there is no vertical strain on the spine. Intervertebral discs degenerate in each individual, with different dynamics.
In the beginning of the disease the space relations in the movement segment are impaired and the segment thus gets into abnormal positions. Such a loosing is called instability.
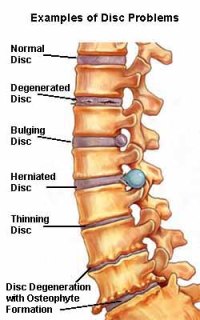
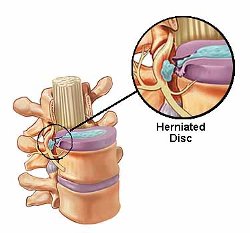
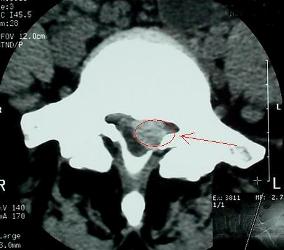
The second phase brings along significant damage of the disc that changes its solid structure, tissues soften and radial fissures occur through which the central soft material may be pushed onto the disc circumference. This phase of disease can develop in the so-called discoradicular conflict, i.e. pressure of the changed disc onto the spinal radix. It is either symmetrical arching of the whole disc - protrusion - when the outer parts of the ring remain unchanged, or prolapse of the disc which is a typical morphological basis of the lumboischiadic syndrome.
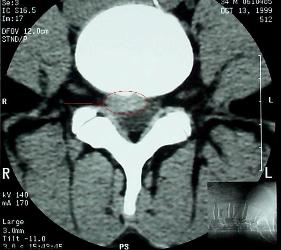
The final phase of the disease is healing reparative changes that result spontaneously in limitation
 of pathological motility in the movement segment. It is based on creation of solid cartilaginous
and, at the end of the healing process, bone tissue. As a result, stability in the impaired movement
segment is renewed. However, an unpleasant consequence may occur - narrowing, stenosis of the spinal
canal, and the so-called osteoradicular conflict may develop when the pressure onto the spinal radix
is given by pressure of solid bone growths. The patient's complaints have also character of LIS.
of pathological motility in the movement segment. It is based on creation of solid cartilaginous
and, at the end of the healing process, bone tissue. As a result, stability in the impaired movement
segment is renewed. However, an unpleasant consequence may occur - narrowing, stenosis of the spinal
canal, and the so-called osteoradicular conflict may develop when the pressure onto the spinal radix
is given by pressure of solid bone growths. The patient's complaints have also character of LIS.
Disc impairment and stenosis of the spinal canal can combine.
Therefore, in some phases of the disease the patient's complaints directly depend on impaired status of the disc, when the spine is challenged, the increased pressure in the disc, the so-called intradiscal pressure, is transferred onto the softened disc circumference which arches and irritates the spinal radix. Reducing the pressure, which should eliminate the radix irritation, is the treatment purpose.
Overview of treatment options
Nowadays, patients have the following treatment options:
- Conservative method
- Micro-surgical operation
- Percutaneous endoscopic operation or operation with automatic tube
- Percutanous laser discectomy
The LIS image has been known since the Hippocrates era but the pathophysiological relations in the spinal canal were explicated only in the 1940s, following the Mixter's and Barra's work in the Mayo clinic in the USA who published their first surgery results and thus started the "disc era".
The first disc surgeries in our country go back to the time before the World War II, and a boom came in the fifties. The Clinic of Neurology in Olomouc belonged to the pioneers of the method. Open major access surgeries with operation on both bone and ligament parts of the spinal canal were now replaced with microsurgical operations that substantially spare all anatomical structures.
Conservative treatment of lumboischiadic syndrome is the basic treatment and saving exceptions, it is suitable for and high-successful in all its forms. The treatment includes various procedures that lead to mitigation of back pain and to relieving of spinal blockage along with pain regression in leg and recovery of impaired functions (limb weakness and sensitivity impairment). Medication treatment in a form of pills, injections and infusions is often the basic element, followed by physical procedures, massages or traction treatment. Semi-invasive procedures involve periradicular therapy (PRT), i.e. application of corticoids under the supervision of a CT device, by which a high concentration of a medicament directly in the affected area is achieved.
An exception that absolutely indicates using a microsurgical operation treatment is the so-called cauda equina syndrome, which is sudden disruption of a disc and massive prolapse of soft tissues into the spinal canal. Sudden compression of nervous structures results in loss of function, with occurrence of limb weakness, urinary disorders and decreased rectal tone. Only immediate surgical loosing of nervous structures can avoid persistent effects.
Microsurgical operation enables safe removal of the disc fragments from the spinal canal, removal of degenerated material from inside the disc, and enables remedy of constricted anatomy via an operation on the bone structures.
 |
 |
 |
Experience in so-called chemonucleolysis, which is reducing the intradiscal pressure via non-standard effect of organic substances - enzymes (papain), led to looking for new surgical methods. Endoscopic operations are now performed through an introduced endoscope with a diameter of ca. 6 mm from one or two inputs, and material from inside the disc is removed either under visual control or using an automatic mechanical tube.
Heating and vaporization effects of laser were used in surgeries of intervertebral discs first time in 1980s. First types of medical-acceptable lasers were used, in particular Ne:Yag with deep penetration into tissues.
It is important to emphasize that the cause of the disease is determined by a disc degeneration which cannot be affected by the treatment.
Physiotherapy plays the crucial role in the treatment of lumboischiadic syndrome. While the functions of the movement segment are impaired, it helps to develop a high quality muscular corset that protects, along with new movement stereotypes, the segment from over-challenge. Physiotherapy is thus of considerable importance at the time of after-treatment, independently of the selected treatment method, and systematic physiotherapy after recovery is necessary for preventative reasons.
Treatment options available for patients these days complement each other and concur, they only compete with each other at some part of the indication spectrum. Each patient thus needs a qualified assessment using imaging methods and a "tailor-made" therapy design. Evaluation of pain is also difficult as everybody feels it differently. At present, decision making by both patient and their physician is influenced by social factors - the pressure of economy with a time factor, i.e. duration of treatment and return to work ability.
The surgery of an intervertebral disc prolapse
The operation technique
After patient identification and verification of the side of operation the patient is get in total endotracheal anaesthesia by an anaesthesiologist and turned into a prone position in a special cradle. Then the height of the impaired disc is marked with regard to bone structures (using an x-ray image of the spine or, in contested cases, a direct checking in an operating theatre using a portable x-ray device. 98 % of prolapses of intervertebral discs occur in last two discs, i.e. L4-5 and L5-S1). A minimal incision through cutis is followed by opening of muscle covers and sequestering of paravertebral musles in the operated segment of the afflicted area and installation of surgical bougie.
Ligamentum flavum is then localised among the vertebral arches which, if covered by a bone due to pathological-hypertrophied intervertebral joints, is exposed using bone instruments or a micro-cutter. The so-called osteoradicular conflict can be resolved by decompression of foramen intervertebrale (foraminotomy). It is increasing of a hole on the bone through which the spinal nerve - radix - gets out of the spinal canal. The ligamentum flavum is then removed, the spinal radix and dura mater are localised and their status is assessed with regard to the disc prolapse that compresses them in order to keep as most epidural fat covering them as possible. When the prolapse capsule is cut through, all fragments are gradually removed under direct visual checking of neural structures. Elimination of decompression in the spinal canal is followed by entering the disc interior through the perforation hole and removing softened tissue which could subsequently penetrate - prolapse - back to the canal. Approximately 25-30 % of the intervertebral disc is removed in total. (The disc overall diminishes by 2-3 mm as late as after a few months and the movement segment is thus stabilized). Absolute control of bleeding, irrigation and in most cases also closure of the surgery incision in two layers follow, the patient is woken up from narcosis and transferred to a post-narcosis room.
Post-operation time
The surgery result is decompression of neural structures. In the period following the surgery it is necessary to establish new stability in the area of the operated segment.
In the evening after the surgery most of patients are able to go to the toilet. Pain in the surgical wound is unpleasant because sequestered axial muscles in the operated segment reacts to each change of body position, but it recedes quickly with analgetization (injections and pills). In most cases, the pain in limb recedes significantly immediately after the surgery. The following day, the patient starts with their individual physiotherapeutical programme under supervision of an experienced physiotherapist. It is progressive challenging with physiotherapeutical techniques which are intended to restore a new muscle balance, avoid bad movement habits and restore, through coordination of mainly abdominal, gluteal and paravertebral muscles, a statodynamic balance in the area of lumbar spine.
The question of sitting is often a subject of controversy. From neurosurgical point of view, the so-called controlled sitting may be allowed immediately after the surgery. The best way how to practice it is to sit straightened up on a typical kitchen chair face to its back, supported by forearms laid on the top edge of the back. Based on protective function of tensioned abdominal, back and gluteal muscles the operated segment is fixed. Relaxed sitting in a soft armchair can be recommended only two months after the surgery, i.e. at the time that the operated segment can be considered to have been cured.
The first week, the patient is hospitalized in a surgery ward; as soon as the suture is removed the further procedures are individual: transfer to the physiotherapy department of the same establishment, transport to a local physiotherapy department or home-care with an individual physiotherapeutical programme. Time to return to work is purely individual depending on the type of job and the patient' status, the course of physiotherapy and the attending physician, and suitability of a spa after-treatment. An average minimum time of stabilization and recovery of the function of the operated segment is approx. 2 months.
Complications as a consequence of the surgical operation are rare, they fluctuate under 1 % and are mostly associated with bad healing of the wound. By involving a direct surgical operation, direct damage of neural and vessel structures is practically impossible thanks to the visual check.
Martin Sameš, M.D., PhD.
Neurosurgeon
